Algorithms and data flow
The algorithm is built up around the treatment-oriented health registry, the Care Pathway Database, which is described in this chapter.
(You will find a figure outlining the Care Pathway Database on this page.)
Personal health data for all patients treated by Helse Bergen are retrieved from the electronic patient records system (DIPS) and stored as a structured dataset in the same format as data variables included in the Norwegian Patient Registry (NPR). These variables are well documented and described, and are understood by all Norway’s health trusts to have the same meaning. This enables other health trusts to easily reuse the same algorithm, since all health trusts have a duty to supply data to the NPR in this format by means of an NPR report.
The Care Pathway Database will give the algorithm access to a large number of episodes, with each episode constituting an admission to a department or the entire hospital stay if the patient remains in only one department. Each episode has associated data variables, such as the date of admission/discharge, gender, age, primary diagnosis, indicators of urgency (elective or emergency treatment) and care level (in-patient/out-patient). The algorithm counts the number of previous primary diagnoses, length of hospital stay, as well as previous readmissions that have taken place before each individual episode. Using this information, the algorithm learns which patients are at high risk of readmission.
When a patient is admitted to the hospital, Helse Bergen wishes to make a prediction about this patient’s risk of readmission. If the risk is deemed high, the doctor will be notified by means of an entry in the patient's notes recorded in DIPS. As time goes by, the patterns underpinning the risk of readmission may change. It is therefore important to put the algorithm through subsequent rounds of training (continuous machine learning) at regular intervals, in order to update it on the basis of the new patient data.
The fully developed algorithm model scores the patient’s likelihood of being readmitted to hospital in the future. A software robot cuts information generated by the algorithm and pastes it into DIPS as an entry in the patient’s medical records. Doctors rely only on the information presented in DIPS, from where they will retrieve any prediction concerning a particular patient.
Treatment-oriented health registry (Care Pathway Database)
The establishment of an internal treatment-oriented health registry (subsequently referred to here as the Care Pathway Database) is crucial if Helse Bergen is to be able to make use of health data derived from the medical records of a large number of patients. Such registries must be warranted in law, cf. Section 6(1) of the Norwegian Medical Records Act, and must meet the requirements for design and organisation set out in Section 7 of the Norwegian Medical Records Act.
Section 2 of the Medical Records Act
Section 2(d) of the Medical Records Act defines a “treatment-oriented health registry” as a “patients’ medical record and information system or other registry, catalogue, etc., in which health data are stored systematically, such that data relating to the individual may be retrieved, and which are intended to provide the basis for medical assistance or the administration of medical assistance to individual people”. Section 8 of the Act imposes a duty on undertakings which provide medical assistance to ensure that they have treatment-oriented health registries.
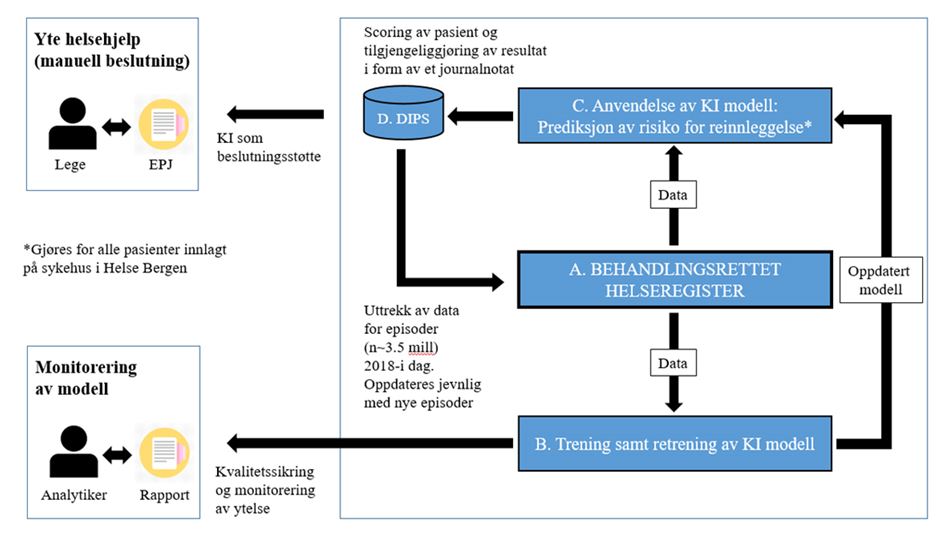
The figure above shows the flow of data in the project:
- A. All data are stored in a treatment-oriented health registry (Care Pathway Database).
- B. The artificial intelligence (AI) algorithm is trained using data from the database.
- C. An updated AI model makes predictions about the risk of readmission for patients admitted to hospital.
- D. The readmission risk prediction is documented in DIPS, is available to the treating physician in the patient’s electronic medical records (EMR) and may be used to support decisions relating to patient care. Patients presumed to have a high risk of readmission may be offered a personalised care package. The quality of the algorithm is regularly assessed and monitored to verify its performance and utility.
Helse Bergen has created several prototypes for the categorisation of patient groups with respect to readmission. Based on NPR data from 2018 to 2020, the project has uncovered several variables specific to individuals, which correlate statistically to the risk of readmission. Provisional results show that by applying machine learning to these variables, it is possible to predict, to an accuracy of 0.75, whether a patient arriving at the hospital will experience a readmission within 30 days. This figure takes into account both sensitivity and specificity, and shows that, in around ¾ of all cases, it will be possible to identify individual patients who will experience or will not experience a readmission within 30 days of their discharge date.
During the autumn of 2022, Helse Bergen will discuss the model's results with doctors who work on a daily basis at the Admissions Clinic at Haukeland University Hospital. In addition, Helse Bergen will work with both clinicians and patients to determine how the results should be communicated in a user-friendly fashion via patients’ notes in DIPS. Efforts will also be made to explore the possibility of trialling the use of PCHTs in a pilot project in a few municipalities.
Helse Bergen considered it necessary to clarify issues relating to privacy and data protection before embarking on any trial of the model in clinical practice.